Artificial intelligence is no longer some far-off concept in a sci-fi movie; it’s a real-world clinical tool that’s actively changing patient outcomes. We’re in the middle of a seismic shift, where algorithms and machine learning models are becoming essential partners for clinicians. Honestly, it feels like we’ve spent decades collecting oceans of medical data, and for the first time, we have a tool powerful enough to navigate them. The numbers back this up: Grand View Research predicts the global healthcare AI market will rocket forward at a compound annual growth rate (CAGR) of 36.4% from 2024 to 2032. This isn’t just about better gadgets; it’s about giving human experts super-vision to spot disease sooner and craft treatments as unique as our own DNA.
The Problem: Drowning in a Sea of Data
Modern medicine is grappling with some immense pressures. Clinicians are facing a daily data tsunami—a flood of high-resolution images, lab results, genomic sequences, and sprawling electronic health records (EHRs). Trying to make sense of it all is like trying to drink from a firehose. This overwhelming volume doesn’t just contribute to physician burnout; it creates cracks where diagnostic errors can slip through. And let’s be honest, the old “one-size-fits-all” playbook for treatment, while a decent starting point, often fails to account for the beautiful, messy reality of individual patient differences.
Key Headaches AI Is Starting to Cure
- The Data Deluge: A single patient journey can spit out thousands of data points. Humans, brilliant as we are, simply can’t connect every faint dot across this vast canvas. AI can.
- Diagnostic Blind Spots: The human eye is remarkable, but it can get tired. It can miss a faint shadow on a scan that signals the beginning of a critical problem. A Johns Hopkins study grimly estimated that medical errors are a leading cause of death in the US—a problem AI is uniquely positioned to help solve.
- The Billion-Dollar Drug Gamble: Traditional drug discovery is agonizingly slow and mind-bogglingly expensive. It’s like searching for one specific grain of sand on every beach on Earth. It often takes over a decade and billions of dollars to get a single new drug approved.
- Reactive vs. Predictive Care: For too long, medicine has been a reactive discipline, treating diseases only after they’ve taken hold. Standard protocols are designed for the “average” patient, but in reality, nobody is truly average.
The AI Co-Pilot: A Second Set of Eyes for Every Clinician
One of the most mature—and frankly, most exciting—areas for healthcare AI is in diagnosis. Here, AI acts as a tireless, data-obsessed co-pilot for the human expert. Think of deep learning models, like Convolutional Neural Networks (CNNs), as digital prodigies. After being trained on millions of labeled medical images, they learn to spot the tell-tale signs of disease with astounding precision.
AI in Radiology: From Overwhelmed to Empowered
Radiology is the poster child for this revolution. And why not? It’s an area defined by massive volumes of standardized visual data—a perfect playground for AI. An AI model can scan a chest X-ray in seconds, flagging a suspicious nodule that a busy radiologist might only see hours later.
Now, let’s bust a myth right here. This does not make radiologists obsolete. It makes them more powerful. The AI acts as a brilliant triage assistant, sorting the massive pile of scans and saying, “Hey, you need to look at these five first.” This frees up the human expert to focus their irreplaceable skills on the most complex cases and, most importantly, on the patient.
A 2024 study highlighted in Nature drove this point home. It found an AI system for breast cancer screening was just as accurate as two radiologists working in tandem. The result? It cut the screening workload by a staggering 44%. This isn’t about replacement; it’s about a powerful human-machine partnership.
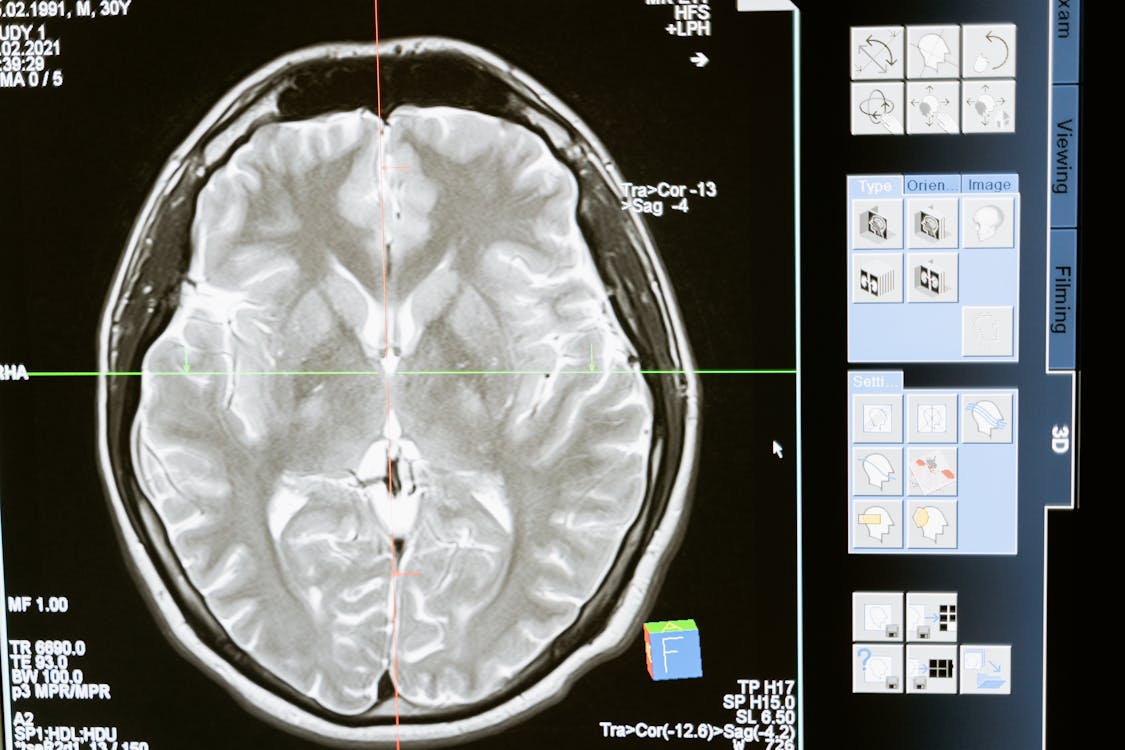
AI algorithms can analyze complex medical scans to detect subtle anomalies that might be missed by the human eye.
Beyond Diagnosis: Treatment Tailored Like a Bespoke Suit
Finding the problem is only half the battle. AI’s role is rapidly expanding into answering the all-important question: “So, what do we do about it?” Standard treatment can feel a bit like offering everyone off-the-rack clothing. It fits some people okay, but it’s rarely a perfect match. Precision medicine, powered by AI, is the equivalent of bespoke tailoring. By analyzing a patient’s unique genetic code, lifestyle, and clinical history, AI can help predict which treatments will be a perfect fit.
- Precision Oncology: A Game Changer: This is where AI truly shines. An AI platform can digest a patient’s tumor DNA, pinpoint the exact mutations fueling the cancer, and then scan a global database of clinical trials and therapies to find the perfect weapon for that specific enemy.
- Supercharging Drug Discovery: AI is turning the slow, expensive process of drug discovery on its head. By predicting how millions of molecules will behave (a puzzle famously cracked by DeepMind’s AlphaFold), AI can identify promising drug candidates in months, not decades. Actually, thinking about it more, this might be AI’s most profound long-term impact. A 2024 report from Boston Consulting Group projects that generative AI could inject up to $110 billion in value into the pharma industry over the next decade.
- AI-Enhanced Robotic Surgery: In the operating room, surgical robots guided by AI are bringing superhuman stability and precision to delicate procedures. These systems create detailed 3D maps, steady the surgeon’s hand by filtering out natural tremors, and even automate repetitive tasks like suturing. The result is less invasive surgery, fewer complications, and faster recovery.
- Crystal Ball for Treatment Response: By learning from the journeys of thousands of similar patients, AI models can now offer a statistical glimpse into the future, predicting how a patient might respond to a particular drug. This allows doctors to be proactive, adjusting a dose or switching strategies *before* a problem arises.
Practical Framework: Let’s Walk in a Patient’s Shoes
To make this tangible, let’s follow the journey of a hypothetical patient named Jane in 2025.
- Step 1: The Proactive Scan. Jane gets a routine chest scan. An FDA-cleared AI tool analyzes it instantly. It doesn’t find anything alarming that needs a radiologist’s immediate attention, but it does spot a tiny, ambiguous area. Cross-referencing Jane’s EHR, it calculates a slight long-term risk and recommends a follow-up in six months—a task that might have been overlooked in a busy system.
- Step 2: The AI-Powered Flag. Six months pass. The new scan shows a change. The AI immediately flags it as high-priority. The radiologist confirms the suspicion. A biopsy slide is then digitized, and a pathology AI not only confirms cancer but also identifies its specific subtype with a level of detail that informs the next step.
- Step 3: Bespoke Treatment Planning. Jane’s tumor undergoes genomic sequencing. An AI platform ingests this complex data. Instead of defaulting to standard chemo, the AI discovers a specific mutation. It then finds a targeted immunotherapy drug—one typically used for a different cancer type—that has an 85% probability of success against this exact genetic driver.
- Step 4: The Guardian Angel Monitor. During treatment, a HIPAA-compliant AI constantly monitors data from Jane’s wearable device and lab results. It detects a subtle pattern indicating a high risk of an adverse reaction, alerting her care team two days before she would have even felt symptoms. They adjust her medication, preventing a serious complication.
The Skills You Need: Becoming a Translator in a New World
The explosion of healthcare AI has created a desperate need for a new kind of professional: a “translator” who speaks both the language of clinical medicine and the language of data science. This isn’t one job; it’s a multidisciplinary field demanding a rare mix of skills.
| Skill Category | Core Competencies | _Why It’s Non-Negotiable |
|---|---|---|
| Technical & Data Chops | Python, TensorFlow/PyTorch, SQL, Machine Learning (CNNs, NLP), Cloud Computing (AWS/GCP/Azure). | These are the hammers and nails. You can’t build the house without them. This is the foundation for creating and deploying models that can wrangle medical data. |
| Healthcare Domain Fluency | Medical terminology, clinical workflows, EHR systems, biology/genomics. | You can’t fix a problem you don’t deeply understand. Building a great tool for a cardiologist requires thinking like one. This is about credibility and effectiveness. |
| Regulatory & Ethical Armor | HIPAA/GDPR compliance, FDA clearance pathways, data privacy, bias detection and mitigation. | This is the most important guardrail. In a field built on trust, navigating the complex regulatory landscape isn’t just a skill; it’s a license to operate. |
| Human-to-Human Skills | Translating geek-speak for clinicians, active listening, project management, ego-free collaboration. | The most brilliant AI is worthless if you can’t convince the doctors to trust it or explain its limits. This is the bridge between the code and the bedside. |
To get started on this path, explore our guides on Data Science and AI Ethics.
The Essential Guardrails: Navigating Ethics, Bias, and Trust
The promise of healthcare AI is dazzling, but we have to talk about the shadows. Its adoption is riddled with challenges that require our full and responsible attention.

Ensuring data privacy and eliminating algorithmic bias are critical challenges for the widespread adoption of AI in medicine.
Key Challenges We Must Confront
- Data Fort Knox: Patient data is sacred. It’s not just about HIPAA compliance; it’s about building fortified systems that are impenetrable to cyberattacks.
- The Ghost of Bias: Here’s a controversial truth: technology is not neutral. If an AI is trained on data from one demographic, it will likely fail others. This isn’t a bug; it’s a feature of poor data strategy that can dangerously amplify existing health disparities. Actively seeking out and destroying bias is job number one.
- The “Black Box” Dilemma: Some of the most powerful AI models are also the most opaque, making it impossible to see *how* they reached a conclusion. This is a massive problem. No doctor can ethically act on a recommendation they can’t understand. This is why the field of “Explainable AI” (XAI) is so critical—it’s about prying open the box and making AI’s reasoning transparent.
- The Regulatory Gauntlet: An AI tool can’t just be downloaded and used. It must survive a gauntlet of rigorous validation. The U.S. Food and Drug Administration (FDA) has already cleared over 700 AI/ML-enabled devices, but getting them to work smoothly and safely within a hospital’s chaotic workflow is its own mountain to climb.
The Human in the Loop: Augmentation, Not Abdication
Let’s be perfectly clear. The fear of AI replacing doctors is a distraction. The only effective and ethical path forward is human-AI collaboration. The AI is the data-crunching workhorse, spotting patterns in the noise. The clinician is the commander, providing critical context, human empathy, and the final, authoritative decision. The future isn’t an AI doctor. It’s a doctor supercharged by AI.
Frequently Asked Questions (FAQ)
Will AI really replace my doctor?
Absolutely not. The expert consensus is firm: AI will augment doctors, not replace them. Think of it as an incredibly powerful support tool that handles the data-heavy lifting, freeing up clinicians to focus on what humans do best: complex problem-solving, patient communication, and providing compassionate care. It’s a partnership, not a replacement.
How accurate is AI in diagnosing diseases?
For very specific tasks, its performance is stunning. In areas like identifying certain cancers on scans or spotting diabetic retinopathy, the best AI models are as good as, or even better than, human experts. But—and this is a big but—its accuracy is entirely dependent on the quality of its training data and the narrowness of the task. It’s at its best when used as a second opinion or a screening tool for a human professional.
What skills do I need for a career in healthcare AI?
You need to be a hybrid. You’ll need a strong foundation in data science and machine learning (Python, TensorFlow, etc.), but that’s just the entry ticket. You must combine that with deep domain knowledge of medicine, clinical workflows, and healthcare data systems. And crucially, you need a rock-solid understanding of the ethical and regulatory rules of the road (like HIPAA and FDA guidelines).
Is my health data safe when used for AI?
Protecting your data is the highest priority. In the U.S. and Europe, any AI application must adhere to ironclad privacy laws like HIPAA and GDPR. Typically, data is anonymized or de-identified, encrypted, and kept in highly secure environments. Newer techniques like “federated learning” even allow models to be trained on data from multiple hospitals without that sensitive data ever leaving its source.
What exactly is ‘personalized medicine’?
Personalized medicine (or precision medicine) is a radical departure from the old one-size-fits-all model. It’s an approach that tailors healthcare—treatments, decisions, everything—to the individual patient. In the AI world, this means using your unique genetic code, lifestyle, and environment to predict your personal disease risks and identify the single most effective treatment path just for you.
Author’s Reflection: The Dawn of a New Medical Age
We’re at the dawn of a new age in medicine, one that will be defined by the “4 P’s”: Predictive, Preventive, Personalized, and Participatory. By finally harnessing the power of data, we are fundamentally shifting from a reactive “sick care” system to a proactive model of genuine healthcare. We can start predicting disease before it happens, personalizing treatments to be maximally effective, and empowering patients to become active drivers of their own health journeys.
The challenges—bias, privacy, regulation—are significant and real. But they are not insurmountable. They are being tackled by a new generation of brilliant, cross-disciplinary professionals who understand that with great power comes great responsibility. The future of health is a beautiful synthesis: the irreplaceable expertise and empathy of human clinicians amplified by the breathtaking power of artificial intelligence. It’s a future that promises longer, healthier lives for all of us.



Leave a Reply